Diagnosis of Heparin-Induced Thrombocytopenia
Complete standardized high quality kit for the diagnosis of HIT
Special features
- Complete kit with ready-to-use components
- Functional Assay
- Non-radioactive method
- Standard equipment and methodology
- Rapid results (<2 hr)
- Patented method
- Registered as Medical Device for In Vitro Diagnostic Use (IVD/CE)
Applications
- Detection of heparin complexes specific antibodies
- Reactivity independent of PF4
- Kit also detects IL-8/heparin and NAP-2/heparin complex antibodies
Introduction
Heparin-induced thrombocytopenia (HIT) is an acute, immune-mediated process that may result in life-threatening thrombosis. HIT is caused by platelet-activating, heparin-dependent antibodies, who form complexes of heparin together with either platelet factor-4 (PF-4) (most of the clinical cases), interleukin-8 (IL-8) or neutrophil-activating peptide 2 (NAP-2). Detection of these antibodies is an important laboratory function.
The antibodies are initially formed after 5 or more days when a patient has been on heparin therapy. An immune response to a heparin dose may be observed within minutes or hours if the patient has had previous exposure to heparin and antibodies are already circulating.
The diagnosis of HIT is difficult because its signs are non-specific and due to the above mentioned structure it is very important to look for the presence and function of the complex specific antibodies.
Diagnostics
For detection of HIT two different kind of assays can be used, the immunological and functional assay. The functional assays reproduce the in-vivo pathophysiology, and highly correlate with the clinical presentation of HIT. This is in contrast to the immune-detection antigen (antigenemia) assays, which measure antibodies reactive to the heparin platelet-factor 4 (PF4) complexes. However, only a fraction of patients positive in these tests develop clinical HIT. On the other hand, pathogenic antibodies may also react with other heparin complexes, such as heparin-interleukin-8, or heparin-neutrophil activating peptide 2, thus, not being detected by those assays.
An immunological assay can be the Enzyme-Linked Immunosorbent Assay (ELISA) or the Gel Test (PaGIA), which is similar to ELISA. The disadvantage of these tests is the fact that they are non-functional assays, they give more than 10% false negative and a 20% disagreement with SRA.
A functional assay is the Serotonin-release assay (SRA), which is sensitive and specific, but non-feasible because of the use of radio isotypes. Another functional assay is the Aggregation Assay but it has a low sensitivity and a long time to perform.
Principle of the HITAlert™ Kit
Recently, the AmericanCollegeof Chest Physicians (ACCP) has posted updates on recommendations for testingof HIT. This should further increase the need of high performance testing for HIT. The HITAlert™ Kit is such a test.
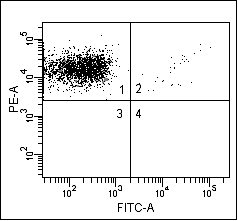
For the HITAlert™ Kit donor platelets (PRP) are used, which are incubated in the presence of patient serum and in the presence or absence of heparin. When pathogenic antibodies are present the activation of the donor platelets is shown using a platelet activation marker. By incubating the samples with an antibody against platelets and the activation marker this reaction can be visualized using flow cytometry.
Results
| A | B | C |
 |
 |
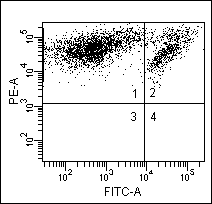 |
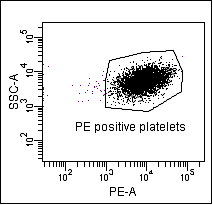
Figure: Results of HITAlert™ Kit: (A) dot plot of PE positive platelets, (B) negative patient, (C) positive patient.
Question: Why can’t you use blood with other additives than citrate (i.e. EDTA, heparin)?
Answer: The platelets can not be activated when using EDTA anti-coagulated blood, because the calcium is depleted by the EDTA. Platelets need calcium for activation. You need a specific concentration heparin to form complexes with PF4. When using heparin anti-coagulated blood the extremely high concentration of heprain will result in an over all negative test procedure.
Question: Can you use blood of a donor with another blood type than blood group O?
Answer: No, it is recommended to use O-type blood so there is no interference of the AB antibodies from the serum sample.
Garritsen et al 2014 IJLH, High sensitivity and specificity of a new functional flow cytometry assay for clinically significant heparin-induced thrombocytopenia antibodies;36(2):135-43.
Solano 2013 HIT Blood Coag fibr, Using HitAlert flow cytometry to detect heparin-induced thrombocytopenia antibodies in a tertiary care hospital; 24(4):365-370
Scully et al 2021 NEJM, Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 nCoV-19 Vaccination, 2021, April 16
